Low FODMAP Diet? What is that and could it help you get to the bottom of your gut or digestive issues?
FODMAP stands for:
Fermentable
Oligosaccharides (oligo –“few,” saccharide – “sugar”)
Disaccharides (“two sugars”)
Monosaccharides (“one sugar”)
And
Polyols (these are sugar alcohols)
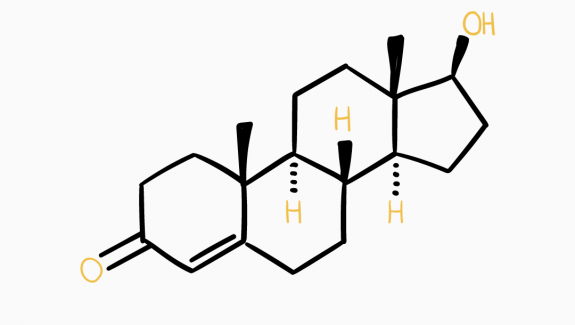
That means FODMAPs are a type of carbohydrate, or “sugar,” found in certain foods. Some people, particularly people with irritable bowel syndrome (IBS) possibly don’t tolerate foods with FODMAPS well or at least some of them only in small quantities. (1)
Essentially a Low FODMAP diet is an elimination diet that you follow for 3-8 weeks which can help you get to the bottom of digestive issues.
In this blog I will explain
→ WHY some higher FODMAP foods might give you stomach pain
→ WHAT the foods are you should avoid and what is safe to eat
→ HOW you go about the diet itself
and finish off with some meal suggestions/recipes you can use while you follow the diet.
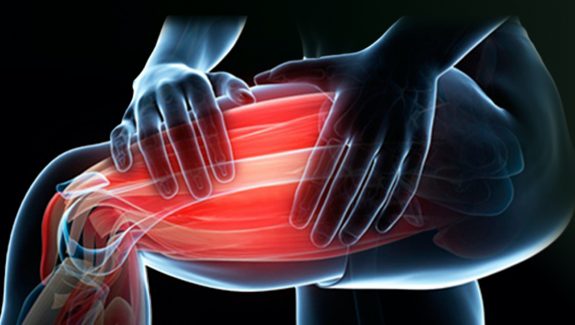
So how come some higher FODMAP foods can cause digestive issues?
The majority of FODMAPs pass through most of your intestine unchanged. They’re completely resistant to digestion and are categorized as a dietary fiber. When they reach your colon, they get fermented and used as fuel by gut bacteria.That also happens when dietary fibers feed your friendly gut bacteria, which leads to various health benefits. BUT, the friendly bacteria tend to produce methane, whereas the bacteria that feed on FODMAPs produce hydrogen, another type of gas, which may lead to gas, bloating, stomach cramps, pain and constipation. Many of these symptoms are caused by distention of the gut, which can also make your stomach look bigger. FODMAPs can also be osmotically active, which means that they can draw water into your intestine and contribute to diarrhea.
So to sum it up, in some individuals, FODMAPs are poorly digested, so they end up reaching the colon. They draw water into the intestine and get fermented by hydrogen-producing gut bacteria, which can lead to
→ Gas
→ Pain
→ Bloating
→ Abdominal distention
→ Diarrhea
Whether your condition goes as far as Irritable bowel syndrome (IBS), a common gastro intestinal disorder, or you are ‘just’ experiencing some of these symptoms occasionally, don’t go believing that this pain is ‘normal’. Get to the bottom of what exact foods or quantities are triggers and this is where a low FODMAP diet comes into play. Gut health is important for more than just well being (check out ou blog on this topic here). It is linked to basically all functions in our body, for example our immune system, our brain, mood…
Before I get into what foods exactly to avoid, let me clarify that in very few cases or only extreme cases of IBS you need to follow a low FODMAP diet forever. On the contrary, some high FODMAP foods actually have great health benefits (cruciferous vegetables, probiotic yoghurt…) and there is no need to deprive yourself of these permanently (check out our blog on benefits of probiotics here).
The idea behind it for most people is to undergo a ‘strict’ low FODMAP diet for a 6-8 weeks in order to give your gut somewhat of a reset and then slowly reintroduce some foods, one at a time, to see what particular ones and what quantity of it caused which symptoms so you can avoid it in the future.
So what food should you avoid and which ones are safe to eat?
Firstly, here are all carbohydrates that are considered FODMAPS:
Fructans and Galactans Polyols, Fructose, Sorbito, Lactose, Mannitol, Fructooligosaccharides Xylitol, Galactooligosaccharides, Maltitol, Fructose. (2)
High FODMAPs to avoid
(Again keep in mind that many foods considered high in FODMAPs are healthy foods otherwise, so don’t mistake them for foods you should generally avoid. (3))
→ Vegetables: Onion, Garlic, Cabbage, Broccoli, Cauliflower, Snow peas, Asparagus, Artichokes, Leeks, Beetroot, Celery, Sweet corn, Brussels sprouts, Mushrooms
→ Fruits: “stone” fruits like Peaches, Apricots, Nectarines, Plums, Prunes, Mangoes, Apples, Pears, Watermelon, Cherries, Blackberries, Dried fruits
→ Legumes and beans: Baked beans, black-eyed peas, broad beans, butter beans, chickpeas, kidney beans, lentils, soybeans and split peas
→ Grains: Amaranth, barley, wheat and rye in highly refined forms such as Breads, Cereals, Pastas, Crackers, Pizza…
→ Dairy products that contain lactose: Milk, Soft cheese, Yogurt, Ice cream, Custard, Pudding, Cottage cheese
→ Some nuts: Pistachios, cashews
→ Sweeteners and artificial sweeteners: High fructose corn syrup, Honey, Agave nectar, Sorbitol, Xylitol, Maltitol, Mannitol, Isomalt (usually found in sugar-free gum and mints, and even cough syrups and other medication)
→ Drinks: Alcohol, Sports drinks, fruit juice concentrate, Coconut water, Chai tea, chamomile tea
Remember that these can also be present in things like sauces and dressings and includes things like breadcrumbs, diet sodas, artificial sweeteners in protein powders etc.
Low FODMAP foods to eat
→ Vegetables: Alfalfa sprouts, Bean sprouts, Bell pepper, Carrot, Green beans, Bok choy, Cucumber, Lettuce, Tomato, Zucchini, Bamboo shoots, Eggplant, Ginger, Chives, Olives, Parsnips, Potatoes, Turnips
→ Fresh fruits: Oranges, Grapes, Honeydew melon, Cantaloupe, Banana, Blueberries, Grapefruit, Kiwi, Lemon, Lime, Oranges, Strawberries
→ Dairy that is lactose-free, and hard cheeses, or ripened/matured cheeses including (If you are not lactose intolerant, you may not need to avoid dairy with lactose.): Brie, Camembert, Feta cheese
→ Beef, pork, chicken, fish, eggs… basically all lean meat and animal products
→ Soy products including tofu, tempeh
→ Grains: Rice, Rice bran, Oats and oat products, Quinoa, Sourdough spelt bread, Bourghur, Buckwheat (kernels, flour) Corn (cob, polenta, tortilla, popcorn, flour), Millet (grain, flour), Sorghum, Wholemeal Wheat, gluten-free bread and pasta (although Gluten is not a FODMAP, but many gluten-free products tend to be low in FODMAPs.)
→ Non-dairy milks: Almond milk, Rice milk, Coconut milk, etc
→ Most Nuts and seed (Almonds and hazelnuts only about 10 or less)
As mentioned, in some cases, portion sizes make a difference as to whether a product has enough high FODMAPs to cause symptoms. For example, a serving of almonds is a good choice that is in these short chained carbohydrates, but eat more, and you could have too many.
When it comes to the benefits of a low-FODMAP diet, the effects have been tested in thousands of people with IBS across more than 30 studies (4).
Evidence from four high-quality studies concluded that if you follow a low-FODMAP diet, your odds of improving stomach pain and bloating are 81% and 75% greater, respectively. Some medical professionals argue also, that a diet that mostly includes low FODMAPs also can help ease symptoms from other health conditions, such as autoimmune diseases (like rheumatoid arthritis, multiple sclerosis or eczema), fibromyalgia or migraines.
It is important to note that the diet, like any dietary change, is an involved process. Therefore, I would not recommend trying it for the first time while traveling or during a busy or stressful period.
So how do you go about it?
Stage 1: Restriction
This stage involves STRICT avoidance of all high-FODMAP foods.
People who first hear of the diet often think they should avoid all FODMAPs long-term, but this stage should only last about 3–8 weeks. This is because it’s important to include FODMAPs in the diet for gut health.
Some people notice an improvement in symptoms in the first week, while others take the full eight weeks. Once you have adequate relief of your digestive symptoms, you can progress to the second stage.
Stage 2: Reintroduction
This stage involves systematically reintroducing high-FODMAP foods.
There are a couple of reasons for that:
- To identify which TYPES of FODMAPs you tolerate. Few people are sensitive to all of them.
- To establish the AMOUNT of FODMAPs you can tolerate.
In this step, you test specific foods one by one for three days each. You need to continue a low-FODMAP diet throughout this stage. This means, even if you can tolerate a certain high-FODMAP food (after you tested it for 3 days), you have to continue to restrict it until stage 3.
It is also important to remember that, unlike people with most food allergies, people with IBS can tolerate small amounts of FODMAPs.
Lastly, remember that even if digestive symptoms can be debilitating, they usually do not cause long-term damage to your body.
Stage 3: Personalization
This stage is also known as the “modified low-FODMAP diet.” In other words, you still restrict some FODMAPs, but the AMOUNT and TYPE are tailored to your personal tolerance, as identified in stage 2. It is important to progress to this final stage in order to increase diet variety and flexibility.
Many people are surprised to find that the low-FODMAP diet is a three-stage process. Each stage is equally important in achieving long-term symptom relief and overall health and well-being, since no one should be living with more restriction than really necessary.
Throughout the process of a low FODMAP diet is helpful to be
→ working with a medical professional, coach or RD to help guide you through the process
→ to closely monitor and track your biofeedback, bowel movements, bloating, fibre, energy etc to actually detect the right triggers
→ tracking your macros to make sure you are still consuming enough calories and the right macros
A low FODMAP diet is the most advised diet for IBS, but the idea of an elimination diet is not new and there are many others for different purposes or conditions out there (check out our blog blog on elimination diets here).
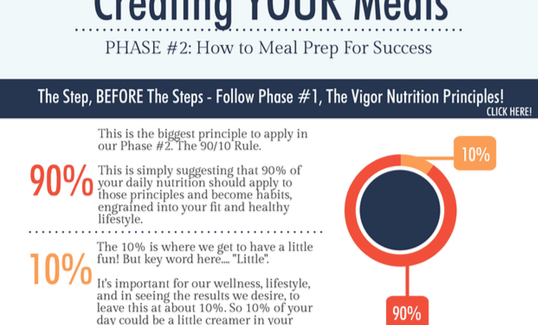
Overall, this diet does not need to be over-complicated though and how you go about assembling your meals does not need to change drastically from what you normally do. Simply pick a good quality protein, add low FODMAP vegetables and then fill the rest with low FODMAP carbs and fats as your macros permit.
Sample Meal Ideas
Breakfast:
→ Overnight oats with almond milk, egg white or soy protein powder (no dairy or legumes), some chia seeds and oat bran, cinnamon and berries or banana (adapted from this recipe).
→ Breakfast Frittata with whole eggs + egg whites, spinach, tomato and turkey bacon on wholemeal sourdough bread (original recipe does not contain egg whites or and asks for prosciutto)
→ Banana Nut Pancakes made with gluten free oats, buckwheat flour, bananas, eggs and almond milk (you can also sub some of the flour for egg white or soy protein powder to increase protein content and decrease carbs, just make sure you increase liquid as well)
→ Peanut Butter and Banana Granola (I would add protein powder to the milk in order to increase protein content or have it with lactose free low fat Greek Yoghurt)
→ Quinoa Berry Breakfast Bake (I would swap 2 of the eggs for egg whites for higher protein content and lower fat)
Soups and Salads:
→ Soups like Carrot, Tomato, Squash, Zucchini, Pumpkin, Sweet potato… prepare with stock, coconut cream or lactose free milk options or with classics like Chicken Noodle Soup opt for rice noodles or swap for wild or brown rice entirely.
→ Salads like this Potato Salad without Mayo (I would swap the bacon for turkey bacon or smoked chicken to increase protein content and decrease fat), or a low FODMAP vegetable mixed salad (I would add Tuna for more protein) or a grain based salad like this Quinoa and Avocado Salad (I would swap the bacon for chicken or turkey).
Mains:
→ Oven roasted mustard chicken with root vegetables (I would swap chicken thighs for breast to lower fat content)
→ Stuffed Acorn Squash (I would swap the quinoa for ground turkey to reduce carbs and increase protein)
→ Brown Rice and Egg Buddha Bowl
→ Turkey Meatloaf (no sugar, no breadcrumbs)
Desserts:
→ Strawberry and Chia Rhubarb Crisp
To sum it up – the low FODMAP diet is an elimination diet that can help you get to the bottom of food intolerances and can therefore help alleviate stomach cramps, pain, bloating and other digestive issues. It is a short term diet (3-8 weeks) that is split into 3 parts – restriction, reintroduction and personalization.
Working with a nutrition coach or dietitian can be helpful when making dietary changes or when trying to get to the bottom of food intolerances.
References:
https://med.virginia.edu/ginutrition/wp-content/uploads/sites/199/2018/05/Low_FODMAP_Diet_12.16.pdf
https://www.health.harvard.edu/diet-and-weight-loss/a-new-diet-to-manage-irritable-bowel-syndrome
https://www.medicinenet.com/low_fodmap_diet_list_of_foods_to_eat_and_avoid/article.htm
https://www.healthline.com/nutrition/low-fodmap-diet#section10
Other linked internal blogs:
http://tailoredcoachingmethod.com/understanding-gut-health/
http://tailoredcoachingmethod.com/elimination-diet/
http://tailoredcoachingmethod.com/probiotics-and-fermented-foods/