Research Review #8
Brandon Roberts, Ph.D., CSCS
Chief Science Officer
Study #1
Title: Wearing of Cloth or Disposable Surgical Face Masks has no Effect on Vigorous Exercise Performance in Healthy Individuals
Question: Is exercise performance impaired by wearing a face mask?
Why
We’ve had our training habits changed by a worldwide pandemic claiming over a million lives. Along with social distancing, wearing face masks is recommended by the World Health Organization. If you’ve spent time in a mask then you know they’re not as comfortable as the Christmas pajamas you’ve been sporting for the last few weeks. However, for the good of society, most people have been wearing them. In fact, some countries wear masks routinely.
Not long after masks were recommended/required, a paper was published hypothesizing face masks could cause complications if worn while exercising. The authors recommended that social exercisers do low to moderate-intensity exercise, rather than vigorous exercise when they are wearing facemasks. The beauty of science is that we test our hypotheses, so a number of papers have been published on the topic of masks and exercise. The current study adds to the literature with the purpose of evaluating whether exercise performance is impaired by wearing different types of face masks.
Who
There were 14 participants with an even split of males and females. They were in their mid to late twenties and normally performed 4-5 hours of moderate to vigorous physical activity per week.
Study Details
The study used a randomized counterbalanced crossover design. Participants completed a progressive cycle exercise test to exhaustion while wearing a cloth face mask, a disposable surgical face mask, or no mask on three separate occasions. Testing was separated by at least 48 hours and each test was at roughly the same time of day.
The starting power output on the ergometer ranged from 35 to 100 watts depending on the fitness level of the participant. The intensity was increased 35 watts every 2 minutes until volitional fatigue, with participants cycling at 70–75 revolutions per minute. During the tests participants were blinded to their performance so that knowledge of their exercise time would not influence subsequent tests.
Results
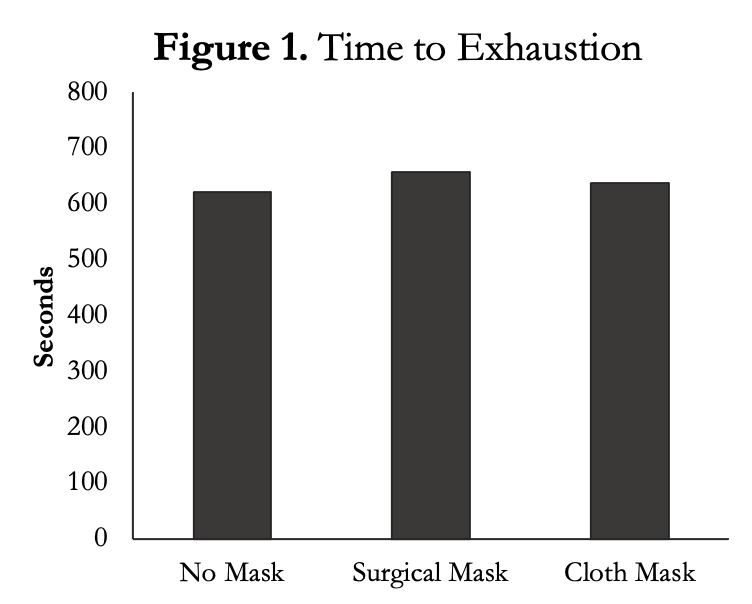
The authors measured time to exhaustion (Figure 1) during the exercise test and found there was no difference between conditions. There were also no sex differences between groups. There were also no differences in peak power during the cycle test (data not shown).
One of the concerns with COVID-19 is oxygenation levels, so the authors used near-infrared spectroscopy (NIRS), which uses infrared light to measure the levels of oxygenated and deoxygenated haemoglobin in blood. The authors found no differences between groups. That means the oxygen delivered into your body is not decreased by wearing a surgical or cloth mask. They also used a pulse oximeter (the thing they put on your finger at the hospital) to measure arterial blood oxygen saturation, which should be somewhere around 95-100%. They found no changes in any of the conditions. This matches the NIRS data and indicates that the amount of oxygen getting into your body is not changed with a mask.
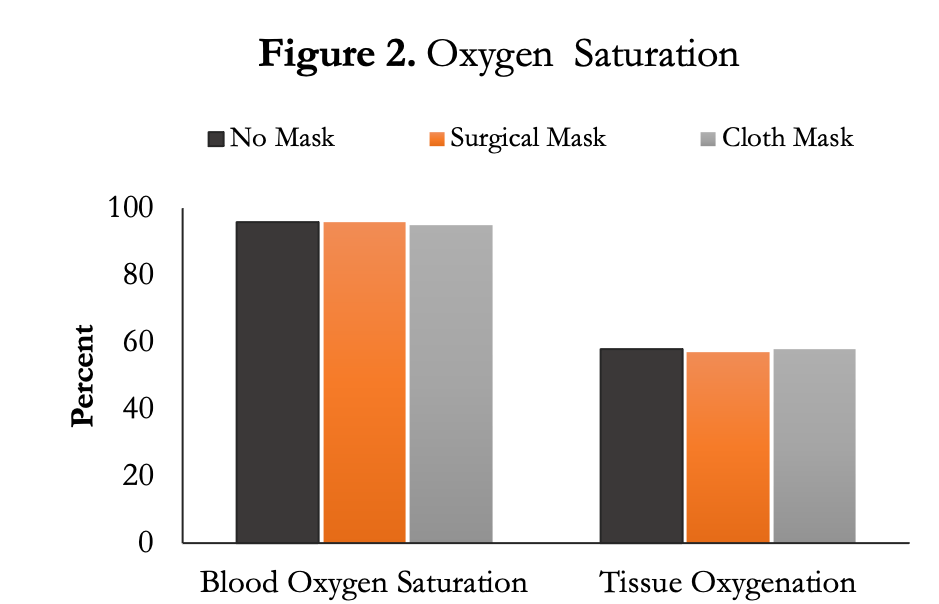
To my surprise, the authors also found that wearing a mask did not change the rating of perceived exertion (data not shown) during the exercise test nor did it change maximum heart rate. All conditions averaged an RPE of 9.6-9.8.
Author’s Answer
“The main finding from this study was that exercise performance, measured as either time to exhaustion or peak power output during an incremental cycle ergometer test, was not affected by wearing either a disposable surgical face mask or a non-disposable cloth face mask. Additionally, face mask and no face mask conditions were not different throughout the exercise test when oxygen saturation was assessed relative to peak power output.”
My Answer
Masks are uncomfortable, especially while exercising. I personally find it much harder to push myself (e.g., HIIT) while wearing one. That doesn’t mean I can’t do it or it’s going to interfere with my workout. The current study supports that idea, finding no differences in exercise capacity or physiological variables when wearing a cloth or surgical mask compared to no mask.
There are two other studies on using a mask while exercising. Fikenzer et al., compared the effects of wearing no mask, a surgical mask, or a N95 mask on cardiopulmonary and metabolic responses. The researchers had the participants wear two masks. The mask they were testing (N95 or surgical) and the one for metabolic measures. The masks for the metabolic measures are fairly uncomfortable already so wearing two masks would make everything harder. The untrained participants then completed an incremental exercise test.
The authors found there were no significant differences between no mask and a surgical mask for all of the performance, pulmonary, and hemodynamic parameters. This indicates wearing a surgical mask won’t make a difference to your body, physiologically, during exercise. However, the N95 mask showed larger negative effects on pulmonary parameters than a normal surgical mask, and both masks significantly reduced forced expiratory volume and forced vital capacity. That’s no surprise because masks are supposed to reduce forward particle velocity, thus lowering the risk of infection for those around you. From this data we can surmise that wearing a surgical mask doesn’t make much of a difference in physiological measures compared to no mask, but N95 masks might lower your performance.
The second exercise study using masks was published by Epstein et al. The authors compared the physiological effects of wearing surgical masks and N95 masks during a short‐term strenuous workout. The authors also used an incremental exercise test on a cycle ergometer. They concluded that ..”short‐term moderate‐strenuous aerobic physical activity with a mask is feasible, safe, and associated with only minor changes in physiological parameters, particularly a mild increase in EtCO2.” The mild increase in end tidal CO2 can be explained by the fact that re‐breathing the expired air that remains within the mask causes mild hypercapnia. Hypercapnia is CO2 retention in the blood and is caused by failure to remove excess CO2 in the body. This could be an issue for people who are unhealthy and can’t adapt — like people with pulmonary diseases — but not for healthy people. A limitation of the study is that the authors used nasal prongs so that participants couldn’t breath out of their nose, which isn’t realistic for using a mask, though does provide scientific validity.
Unlike the previous two studies, the benefit of the current study is that it mimics what we do in the gym. Most people wear cloth or surgical masks, not N95s. The limitation to this study, and others referenced above, is that they’re testing maximal effort. When you’re going to the max nothing is comfortable. Yet, we seldom exercise at a maximal capacity. So we don’t know how a mask does or does not change a typical 30-90 minute workout in the gym. I would hypothesize that RPE might slowly increase over time. Another major limitation is this study started in September by which most people had probably adjusted to wearing a mask. The authors should have asked a few simple questions about the participants’ history of wearing a mask while exercising. Since these people had been exercising for 4-5 hours a week they probably had worn a mask for some of it and there may be some type of mental adaptation that occurs over time.
How can we apply this?
We can understand that wearing a mask, while uncomfortable, doesn’t hinder our workouts on a physiological level or put healthy people at risk of having oxygen deficits.
What’s next?
At the time of this article two vaccines have been approved for COVID-19, so hopefully we won’t have to deal with masks too much longer. However, a simple next step would be to do a full workout or a few weeks of training in a mask to see if there are any differences with training adaptations over time.
Study #2
Title: Estimating Repetitions in Reserve for Resistance Exercise
Question: Does knowing the weight on the bar influence your RPE?
Why
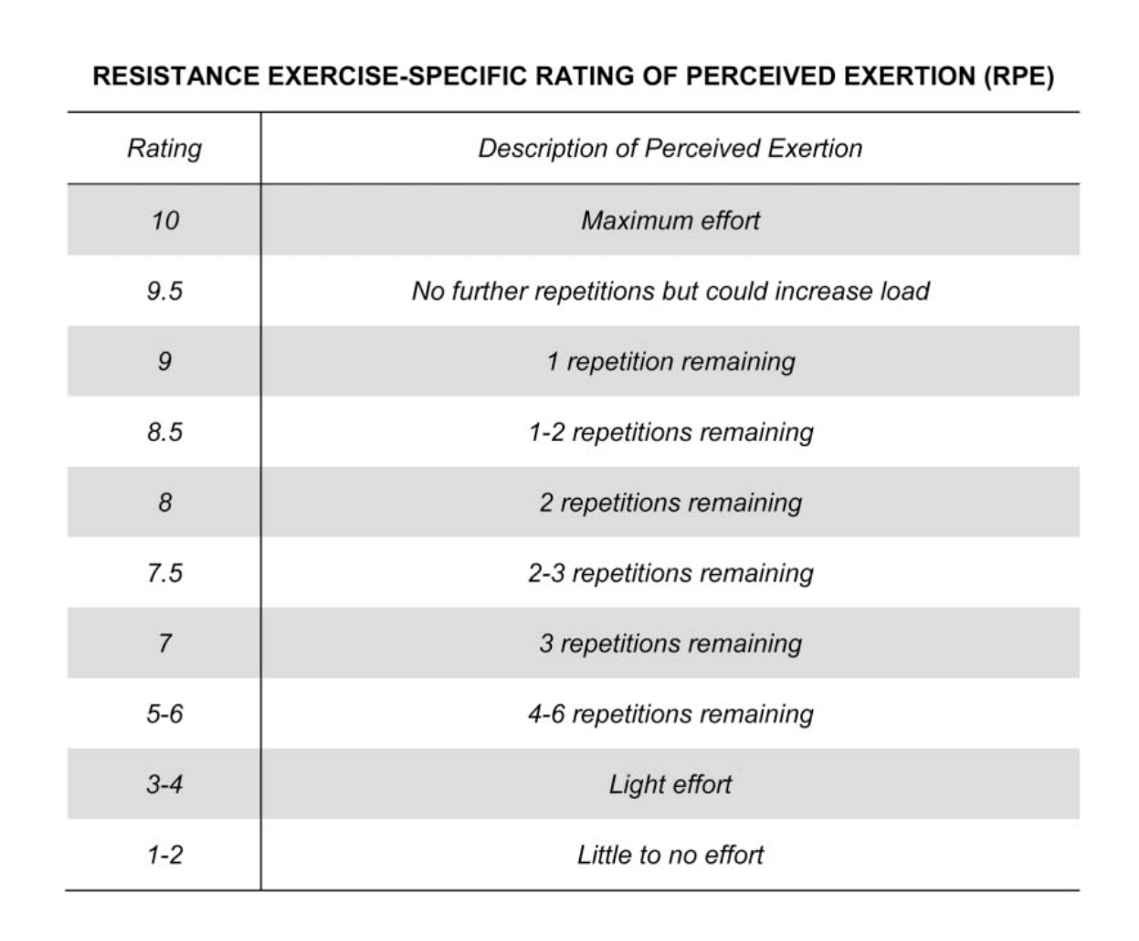
The first study on rate of perceived exertion (RPE) with repetitions in reserve (RIR) was published a mere five years ago, but the idea was established long before that by Mike Tuscherer (2008). This programming method shifts away from reps and sets based on the percentage of 1RM and towards autoregulation. One of the main reasons we might want to not use 1RM based training is so that we don’t actually have to do 1RM testing. Most people don’t need to do 1RMs (including athletes) and they can also increase the risk of injury. We also have day-to-day fluctuations in how we’re feeling, so autoregulation methods give us a method to adjust training quickly.
The RPE/RIR scale was, in part, inspired by the estimation of reps to failure (ERF) scale. ERF is based on a simple inverse scale, where the ERF number corresponds to the reps to failure.
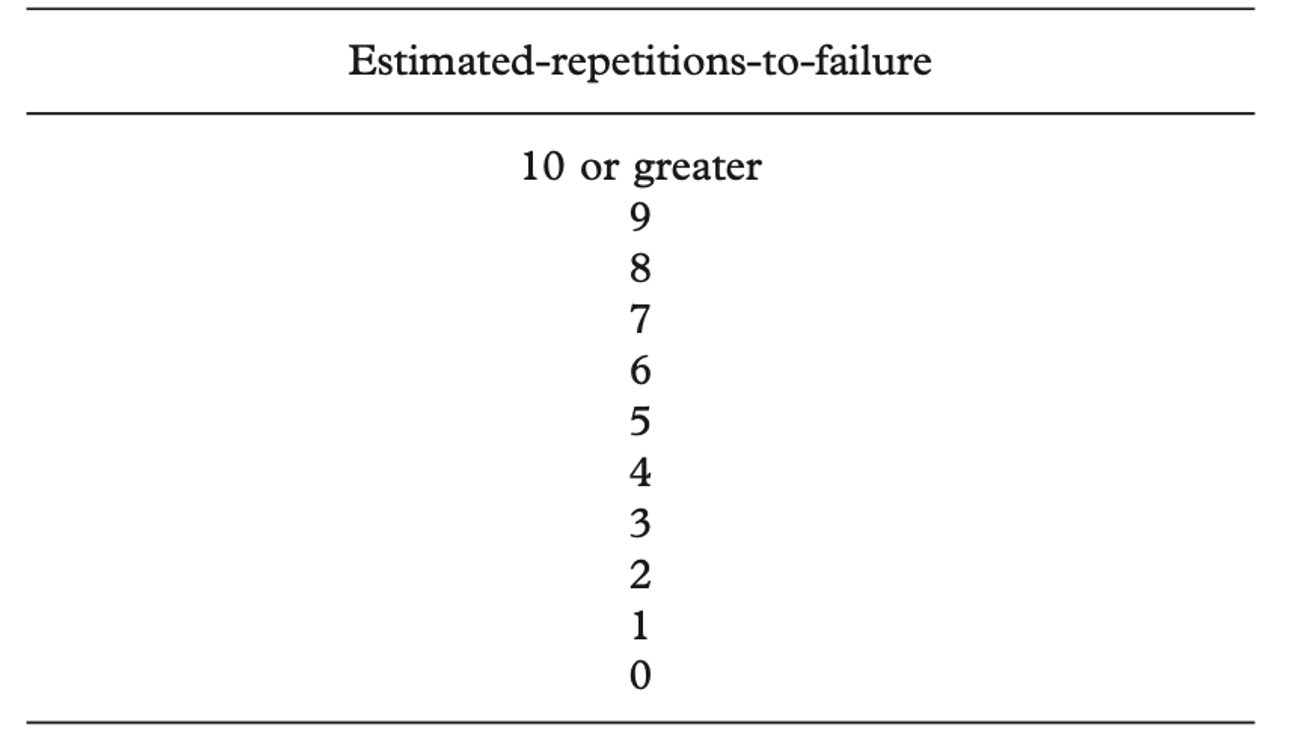
In the first study on ERF, RIR were given by bodybuilders during a 70% 1RM set, then participants continued to failure to see how close they were to their estimation. The authors found strong positive correlations between estimated- and actual-repetitions-to- failure across all participants. Interestingly, participants underestimated reps to failure by ~1 during the first set and accurately predicted reps to failure on the subsequent sets. Therefore, the ERF scale was found as a useful tool in predicting effort and could be useful to assess effort during sets when not going to failure, and could help with the planning of training.
The first study on the RPE/RIR scale was published by Zourdos et al in 2016.. The primary aim of that study was to compare RPE/RIR at different intensities of 1RM in experienced and novice squatters. There was a strong inverse correlation (r = -0.88) between average rep velocity and RPE/RIR. They also found that RPE aligned with 1RM with 94% of experienced squatters giving an RPE of >9.5 at their 1RM. This data indicates that RPE/RIR is a good measure of intensity.
RPE/RIR faced an obstacle shortly after it was created. A massive study (n = 140) showed that people underestimated RPE/RIR by 2-3 reps. The problem with this study was that the participants only did a single set to failure and they weren’t familiar with the RPE system. Another study by Zourdos et al., found that being farther from failure and having high rep sets are associated with more inaccurate predictions of RPE/RIR. This begs the question: are there any other circumstances that can influence RPE/RIR?
The primary goal of the current study by Mansfield et al., was to determine whether the accuracy of RIR estimates for trained individuals is influenced by knowing the load being lifted. A secondary aim was to examine whether the accuracy of RIR estimates is affected by the actual load being lifted (60 vs. 80% of 1RM).
Who
There were 20 healthy men with an average age of ~25 who weighed about 86.5kg. All of the participants were trained and completed at least 2 sessions per week for 2 years. They had no prior experience with the RPE/RIR system.
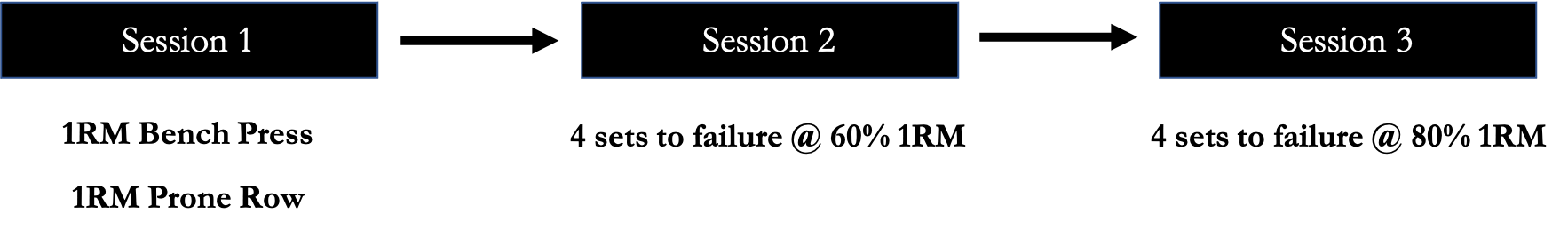
Study Details
The study was a mixed design. There were between-subject comparisons to determine the effect of blinding the load lifted. There were also within-subject comparisons to determine 60% and 80% of 1RM bench press and prone row.
The participants in the nonblinded group were told the amount of weight added to the bar and how many repetitions they could expect to complete at the load, based on estimates from established calculations. Participants in the blinded condition were not told either weight or expected reps. Cardboard screens were placed on both sides of the barbell and the weights were wrapped in a black bag to prevent participants in the blinded condition from seeing how much they were lifting.
The authors estimated that participants could complete ~15 repetitions at 60% 1RM and 6-8 repetitions at 80% 1RM based on previous research. However, when they did pilot testing they found that the maximum number of reps per set declined over time. If you’ve ever gone to failure on multiple sets this has probably happened. You can do 15 reps, then 13 or 12, etc., if you don’t decrease the weight.
During the 60% and 80% testing phase, participants were asked to estimate RPE/RIR on the 8th repetition during the 60% protocol and on the 3rd repetition on the 80% protocol.
Results
There was no difference in blinding and not blinding participants on any of the outcome measures. Therefore, the groups were combined in the analysis. This tells us that it doesn’t matter if you know the load on the bar for RPE/RIR accuracy.
When the authors compared estimated to actual RIR the greatest difference was during the first. At 60% of 1RM bench press the estimates were off by a whopping 7 reps. The participants rebounded quickly because the next set they were only off by 1-2 reps and there was no statistical difference between estimated and actual RIR. They were much closer to estimating RPE/RIR with the 80% 1RM bench press, but still off a few reps on the first set.
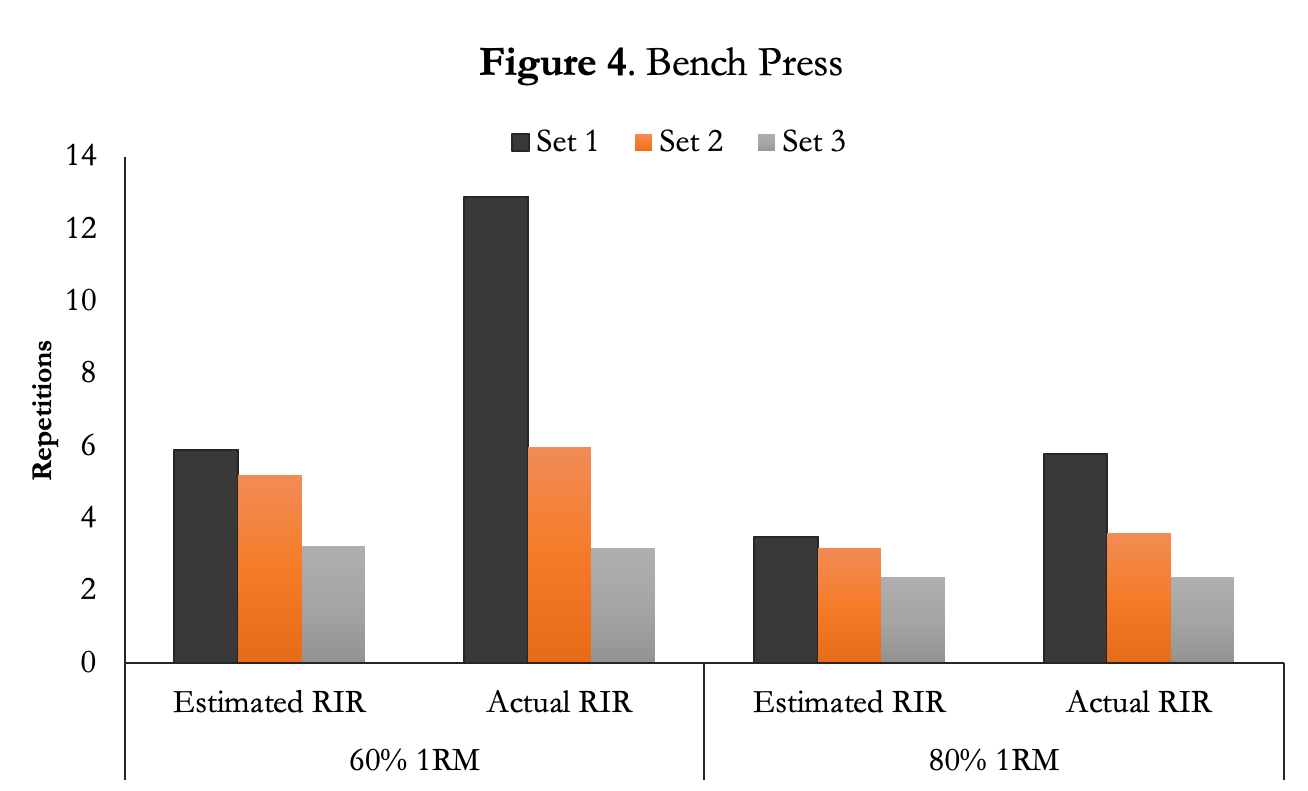
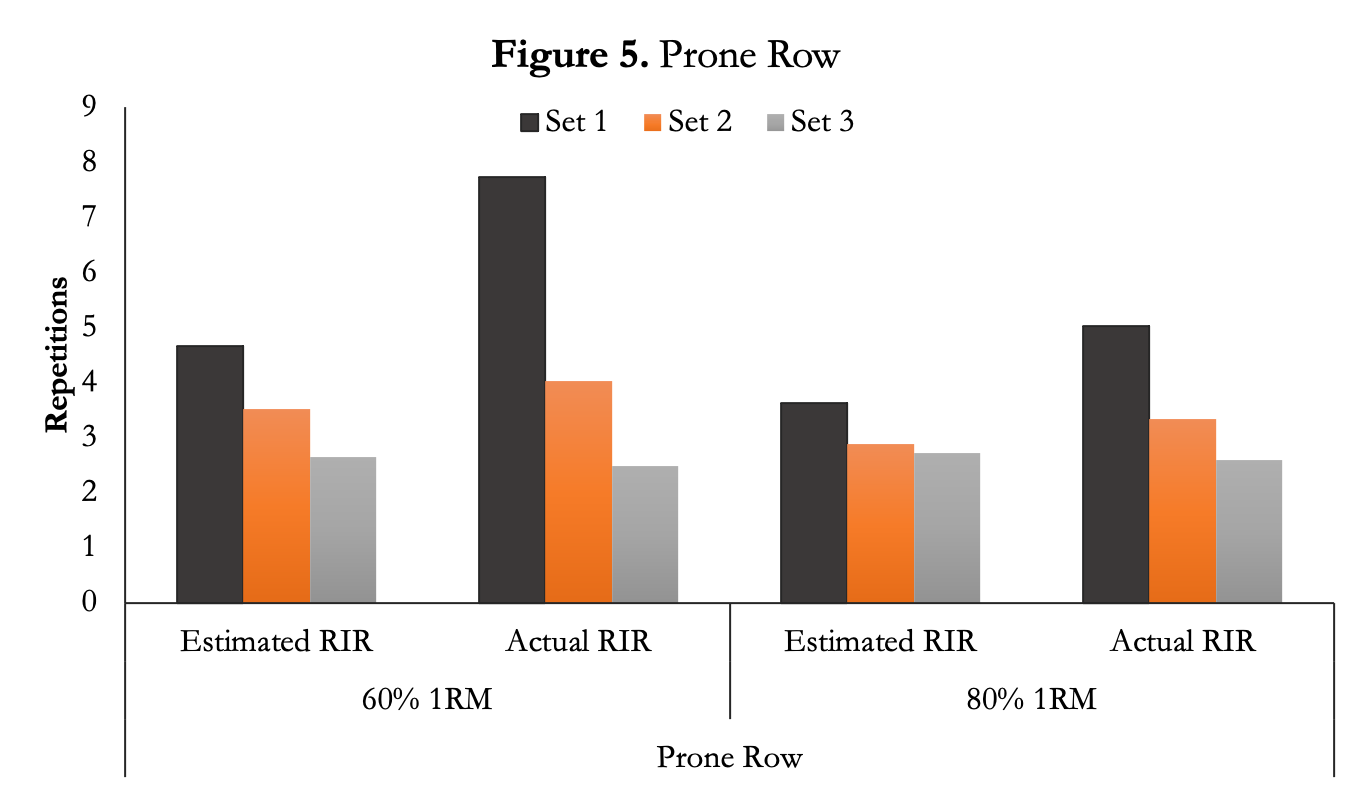
Likewise, the authors compared estimated to actual RIR with the prone row. The greatest difference was during the first set for both 60% and 80% of 1RM. Afterward, the estimated and actual RIR was roughly the same for the second two sets.
Author’s Answer
“Our investigation shows that use of theRIR method is not influenced by the athlete’s knowledge of the load being lifted during a set and therefore is a viable strategy of autoregulation able to be used in resistance training.”
My Answer
RPE/RIR was built on the idea of estimating 1RM without actually doing one. Then researchers pivoted to using it for autoregulation. That seems reasonable because the rate of recovery from training and the rate of adaptation are individual, so RPE/RIR gives us an easy way to control what we do in the gym depending on how we’re feeling.
The current study wanted to know if seeing the weight on the bar influences the number of reps you do at a certain RPE. It doesn’t. Covering the weight on the bar may seem odd, but powerlifters have used this method for a long time to help them get past the mental blocks that occur with training. For example, if you’ve failed a 500lb squat multiple times, it may be in your head that you’re going to fail every time you try something at or above 500lb. There’s a whole field of sports psychology research that studies how athletes think about performance. The other component of covering the weight is that participants don’t have an anchor to how many reps they think they can do, so they wouldn’t be inspired to “beat the log book” to show progression.
The authors hypothesized that individuals would be more accurate with their RIR predictions when using 80% of 1RM over 60% of 1RM. They were correct, but the difference mainly occurred during the first set and not the second or third set. That might be because participants are fresh during the first set. As I mentioned in the intro, the first set seems to be the hardest to predict reps to failure.
The other factor is these participants have never used the RPE system. If they ended up using weights they’ve never used in the gym it would be harder to predict reps. For example, let’s say my bench press max is 275lb. The 60% set would be at 165lbs and the 80% set would be at 220lb. There’s a good chance I don’t train with those exact numbers, so knowing them before I complete my set doesn’t help me predict my reps much.
In the introduction I walked you through the progression of how RPE/RIR has been studied in the last few years. To little surprise, we’re slowly learning more over time. The field has also started to compare RPE/RIR based training to other styles. For example, Helms et al., recently demonstrated that RPE/RIR load prescription resulted in greater back squat and bench press strength over 8 weeks than percentage-based load prescription in well-trained males. This makes a good case for using RPE for people who don’t need to 1RM (aka most people).
How can we apply this?
We can use the RPE/RIR system and know that you can complete the most reps on the first set. Training to failure prolongs recovery time vs. nonfailure training, which could lead to diminished training frequency and volume. Using the RPE/RIR scale can help prevent training to failure if you can accurately predict where you’ll fail.
What’s next?
It would be interesting to see how accurate RPE is over the course of an entire workout, or repeated workouts, rather than a few lifts. Do we get less accurate the more fatigue we accumulate? On a different note, does the environment matter – like if we’re listening to music does that change our RPE/RIR?
Before you leave this month’s Research Review, know that we have multiple ways of consuming this content! So if you’d rather watch or listen, check out the video and audio below this text! We have them available in all three formats, every month:
[Also available via iTunes and everywhere else Podcasts are available]