*Note from Brandon: if you want to learn how to interpret research go read each study before reading the breakdown below, take notes, then compare your interpretation to mine.
[Rather listen to this Research Review? No problem, use the player below or tune in where-ever podcasts are available!]
Study #1
Title: Heat and cold therapy reduce pain in patients with delayed onset muscle soreness: A systematic review and meta-analysis of 32 randomized controlled trials
Question: Does heat or cold therapy reduce DOMS?
Why
Delayed onset muscle soreness (DOMS) is the feeling of pain or discomfort in your muscles after a workout. It mostly occurs after unaccustomed exercise, and normally increases in intensity in the first 24 hours after exercise, peaks from 24 to 72 hours, then subsides in a few days. I wrote my first article about DOMS roughly five years ago, and a lot of data has been published since then. The current hypothesis is that microtrauma and subsequent inflammation inside the muscle causes DOMS.
That’s well and good. How do we make the pain stop? That’s the important question. To alleviate the symptoms of DOMS, some reach for non-steroidal anti-inflammatory drugs, which we covered in a previous research review. That could be detrimental if done for too long at high dosages. Others may try stretching, but according to a Cochrane Review (gold standard) the evidence from randomized studies suggests that stretching before, after, or before and after exercise, does not reduce DOMS in healthy adults. Another option is transcutaneous electrical nerve stimulation (TENS), but that doesn’t seem to work either.
The current study is a systematic review and meta-analysis. I don’t usually cover these in my research reviews, but they serve as a good overview for a body of literature if it is large enough. The purpose of this study was to review and meta-analyze Randomized Controlled Trials (RCTs) that evaluate the effect of heat and cold therapy for the treatment of DOMS. In addition, the authors wanted to identify the most effective method to help patients with DOMS.
Who
A total of 32 RCTs involving 1098 participants were included in the analysis. The average age wasn’t directly reported, but most studies had participants in the 20-30 age range, with one study with participants who were 70-80 years old.
Study Details
The study was pre-registered on PROSPERO. The outcomes in the pre-registration match those reported in the study, so the authors didn’t pull any fast ones.
At least one outcome measure of muscle soreness and/or muscle damage were reported in all of the studies. DOMS was measured by pain score of a visual analogue scale (VAS), a muscle soreness questionnaire, a Likert scale or a modified Talag scale. Only outcome variables measured at the baseline (pre-exercise) and post exercise were included.
Types of cold and heat therapy included cold or hot packs, cold water immersion, cold therapy, infrared radiation, and ice massage. There were a lot of different components going on here. That doesn’t bode well.
Likert scales are a standard outcome science. The scale is named after Renis Likert (1903–1981). A Likert scale is generally a five or seven point scale that ranges from “strongly disagree” to “strongly agree”. You’ve probably seen these before.
A visual analog scale (VAS) is a tool used to help a person rate the intensity of certain sensations and feelings, in this case as pain. The scale for pain is a straight line with one end meaning no pain and the other end meaning extreme pain. A patient marks a point on the line that matches the amount of pain he or she feels. It’s then measured, usually in millimeters, to compare groups. The Talag scale is similar to a VAS scale.
Results
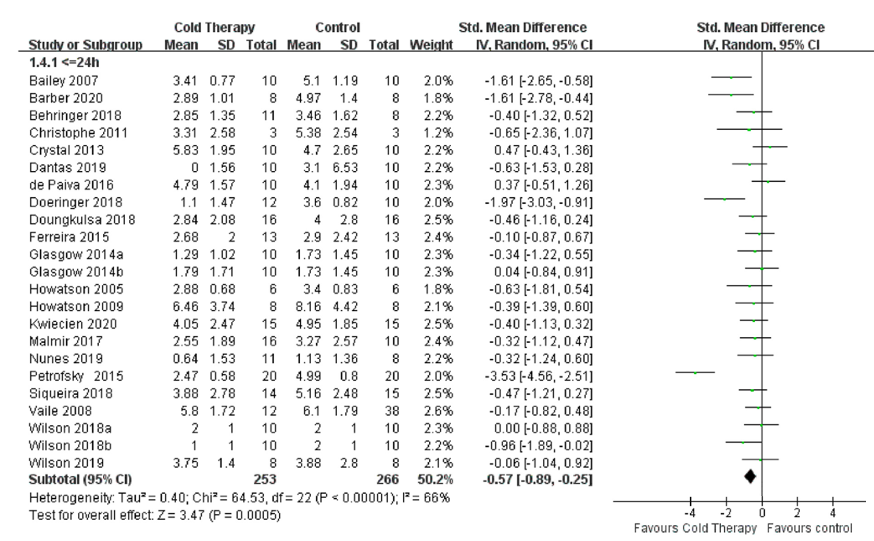
Overall, there were 22 studies analyzed for the effects of cold therapy on DOMS. The authors split them into two categories: ≤24 hours and >24 hours. The figure below is a forest plot, comparing cold therapy versus control. Each horizontal line on a forest plot represents a separate study being analyzed, with the name of the study on the far left and the mean difference on the far right. The green dot on the horizontal line is the mean. If a line crosses the 0 axis, it does not have an effect. If you want a full tutorial on how to interpret these graphs click here.
Figure 1. Forest Plot of Studies that compared cold therapy to control ≤24 hours post-exercise.
In the ≤24 hours analysis there was a significant effect favoring cold therapy. This is visualized by the black diamond at the bottom, and if we look at the bottom left we see that p < .05 so the effect is significant. This effect was mostly driven by four studies: Bailey et al., 2007; Barber et al., 2020; Doeringer et al., 2018; and Petrofsky et al., 2015. Keep those in mind for later. We’ll look at why they might have such a strong effect when the others don’t. Let’s look at >24 hours next.
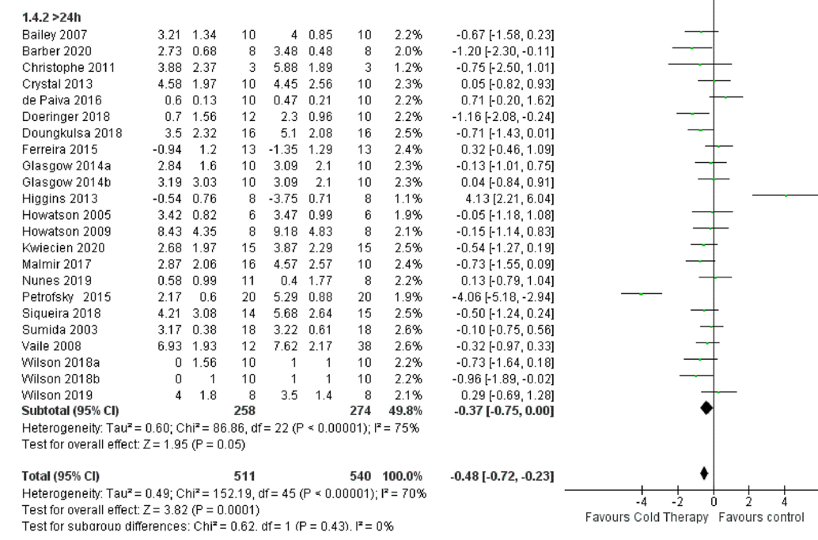
Figure 2. Forest Plot of Studies that compared cold therapy to control >24 hours post-exercise.
As we can see, there are a few strong studies pulling in opposite directions, but most studies cross the 0 point on the axis, which means they are not significantly different. The two studies on opposite ends of the spectrum are Petrofsky et al., 2015 and Higgins 2013. We’re definitely going to take a closer look at the Petrofsky study now.
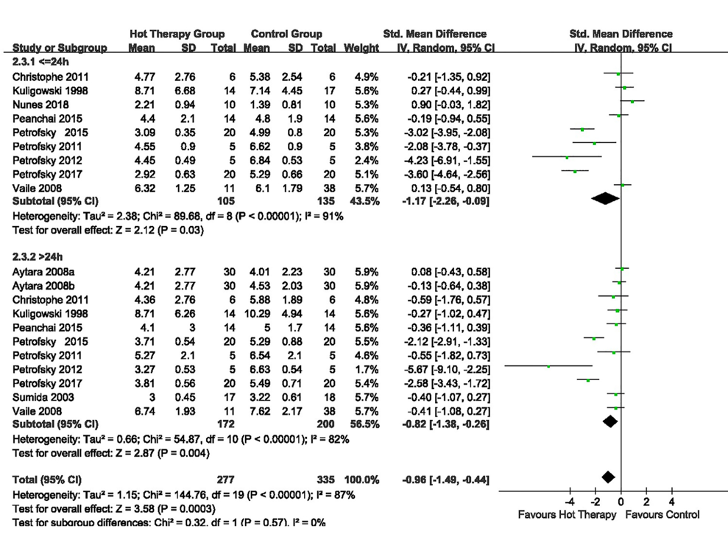
Moving to the heat therapy forest plot we see a significant effect for both heat applied ≤24 hours and >24 hours post-exercise. The ≤24h data is a little more convincing here. There is a slight concern with the same author having such strong effects (Petrofsky again).
Figure 3. Forest Plot of Studies that compared heat therapy therapy to control ≤24 hours and >24 hours post-exercise hours post-exercise.
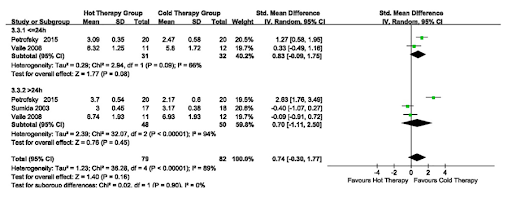
Now, what if we compare the two therapies? The authors did that and found that there was no significant difference. However, only 5 studies were able to be included.
Figure 4. Forest Plot of Studies Comparing Cold vs Heat Therapy.
Author’s Answer
“The present evidence suggested that both heat and cold therapy may facilitate recovery and alleviate pain of DOMS patients effectively within the first hour after exercise. The results also demonstrated that cold treatment can lower the level of pain within 24 hours after exercise, while hyperthermia has an effective impact on reducing pain within 24 and more than 24 hours post-exercise.”
My Answer
The authors got it right based on their analysis of the data. They found that cold treatment and heat therapy work, especially if given within 24 hours. Neither one works better than the other although there weren’t many studies that compared them directly. These results don’t tell us too much though. We have no idea how to apply the cold or heat. Nor do we know how long to apply it for. We just know that it probably needs to happen on the first day after exercise to have the best effect.
The rationale for using heat therapy is that it stimulates blood flow and metabolism in the muscle. Furthermore, it can facilitate special molecular events like mitochondrial biogenesis and heat shock proteins. It activates calcium channels in nerve and skin cells, allowing an influx of calcium into the tissue. Calcium then inactivates pain receptors. Heat also increases the basal metabolic rate in tissue, which promotes healing. Hot water immersion, hot pack and ultrasound are all methods of heat therapy that have been widely used. All three of these were included in the meta-analysis.
The purpose of using cold therapy is to reduce swelling and slow the metabolism so that chances of injury are reduced. Cold also reduces pain by slowing down the never conduction speed. Ice packs, cold water immersion (CWI) and cryotherapy are all methods of cold therapy after exercise. Ice packs affect the muscle by decreasing the intramuscular temperature, thus decreasing the levels of metabolites in the tissue. On the other hand, CWI and cryotherapy decrease core temperature while also decreasing intramuscular temperature. Cryotherapy is the most recent of the post-exercise techniques to be introduced and involves exposure to extremely cold temperature (−148°F) for only a few minutes. The theory is these extreme temperatures will stimulate the sympathetic nervous system, which will reduce muscle metabolism, microcirculation and nerve velocity, thus leading to a change in cytokines and cell signaling.
A number of studies have confirmed that both heat and cold therapy have the effects of alleviating DOMS. One of the studies that sticks out in this meta-analysis is Petrofsky et al., 2015. The authors recruited a hundred subjects to do bodyweight squats for 5 minutes at the speed of 1 squat every 3 seconds. They rested for a few minutes, then did two more sets. I’m not sure about you, but that’s not really a workout I’m going to do. To add, these participants were untrained and had no training in squats. It does provide a decent proof of concept though. The groups were (a) control, (b) cold pack immediately after exercise, (c) cold packs applied 24 hours after exercise, (d) heat packs applied immediately after exercise, and (e) heat packs applied 24 hours after exercise. For cold wraps they used ThermaCare cold wraps directly on the skin for 20 minutes, and for heat treatment, they used ThermaCare heat wraps applied for 8 hours to standardize the heat and cold application. The authors found that cold therapy was slightly favored over heat therapy (see figure with comparison in meta-analysis) and was best if applied immediately post-training.
Another study strongly affecting the analysis [Figure 1] was Doeringer et al. The goal of this study was to assess the impact of CWI on post-exercise recovery in athletes, by evaluating pain perception and muscle performance measurements including strength, power, flexibility, agility, and speed. CWI consisted of immersing their entire lower body to the pelvis in a 70-gallon rubber tub for 15 minutes. The water was consistent at 50°F (10 °C) for each subject. The authors found that strength increased, agility improved, and pain/soreness was reduced in the groups that were exposed to CWI immediately following exercise. However, flexibility, power, and speed were unaffected by CWI.
The two studies above are perfect examples of how cold therapy can work, but using completely different methods. It would be much easier to apply an ice pack for 20 minutes than immerse yourself in a cold tub after training. This leads us to an important point. Not all meta-analyses are good. That’s because they need similar studies for a proper analysis. The main issue with this analysis is they combined too many dissimilar studies. In fact, I’m not sure this study does more than point us in the direction of other important studies we can analyze that show strong benefits with clear methods.
How can we apply this?
If you have problems with DOMS, it might be worth trying heat or cold post-exercise. I would opt for heat therapy, such as a warm pack for a few hours, rather than something cold like an ice bath, especially if your focus is on hypertrophy.
What’s next?
There are a few scientists who are focusing on this line of research extremely well, such as Petrofsky. I think redoing this analysis with more stringent criteria would be a good next step.
Study #2
Title: Observational Study of Lipid Profile and C-Reactive Protein after a Seven-Day Fast
Question: How does a one week fast affect health?
Why
If you look around the internet you can probably find information on fasting. There are claims that it can help everything from cognition to autophagy. Some of these claims are based on evidence in healthy, obese, and even people with diseases like cancer or diabetes. So, it must be good for us, right? In this research review I will walk you through the science behind fasting using a recent study that was published. We’ll start with the question you should always focus on in the fitness world – is it safe? Then, we’ll weave through the literature to see what exactly happens during fasting, and then compare it to some other dieting methods.
The purpose of the current study was to assess the effects of a one-week periodic fast on selected markers of good health. The primary outcome was the effect on the LDL, assessed before the fasting period then again two months later. The secondary outcome was to assess short-term effect on LDL, measured right after the end of the fast, and its short-term and lasting effect on other blood measurements, clinical parameters and body composition.
Who
41 people who attended the facility were eligible to participate in the study. The participants were, on average, 50 years old. They weighed ~73.5kg and had a BMI of 25.5, which is at the low end of the overweight category.
Study Details
This study was pre-registered.
Data was collected during an observational study in a non-medical fasting center in Switzerland, where the participants fasted for one week and undertook physical activity and stress management (e.g., walking, Pilates, yoga, and painting), under the supervision of naturopaths.
The diet consisted of diluted fruit juices in the morning and vegetable and miso broths in the evening, reaching a maximum total intake of approximately 300 kcal per day. Frequent hydration with water and infusions was recommended.
Physical activity was light, rarely moderate and voluntary. Some participants underwent colonic irrigation before starting the fast in a distinct health center.
The data for day 1 includes 40 participants.
The data for day 7 includes 39 participants.
The data for day 60 include 36 participants.
Body composition was measured via bioelectrical impedance (BIA). Blood was analyzed for glucse, cholesterol (HDL/LDL), triglycerides, C-reactive protein and IGF-1. Clinical parameters, such as blood pressure, heart rate, body weight and circumference values were also measured at each timepoint.
Results
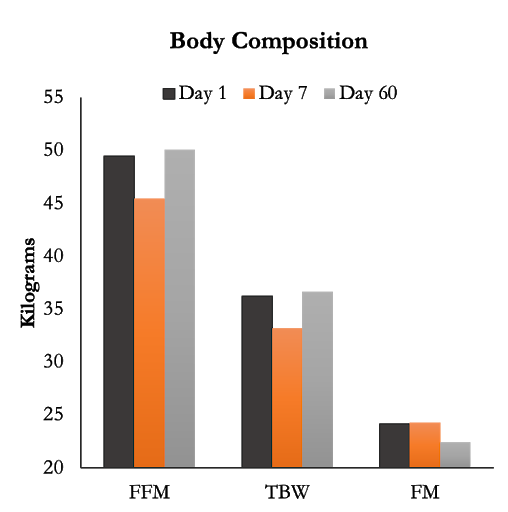
Seven days of fasting significantly reduced fat free mass by 3.84kg, total body water by 2.81kg and did not significantly change fat mass. These results shouldn’t be a huge surprise because the participants are mostly using their glycogen and intramuscular fat stores during the fasting period. If we look farther out, on day 60, all measures had returned to normal, but fat mass decreased by a significant 2.93kg while fat free mass was significantly increased compared to day 1.
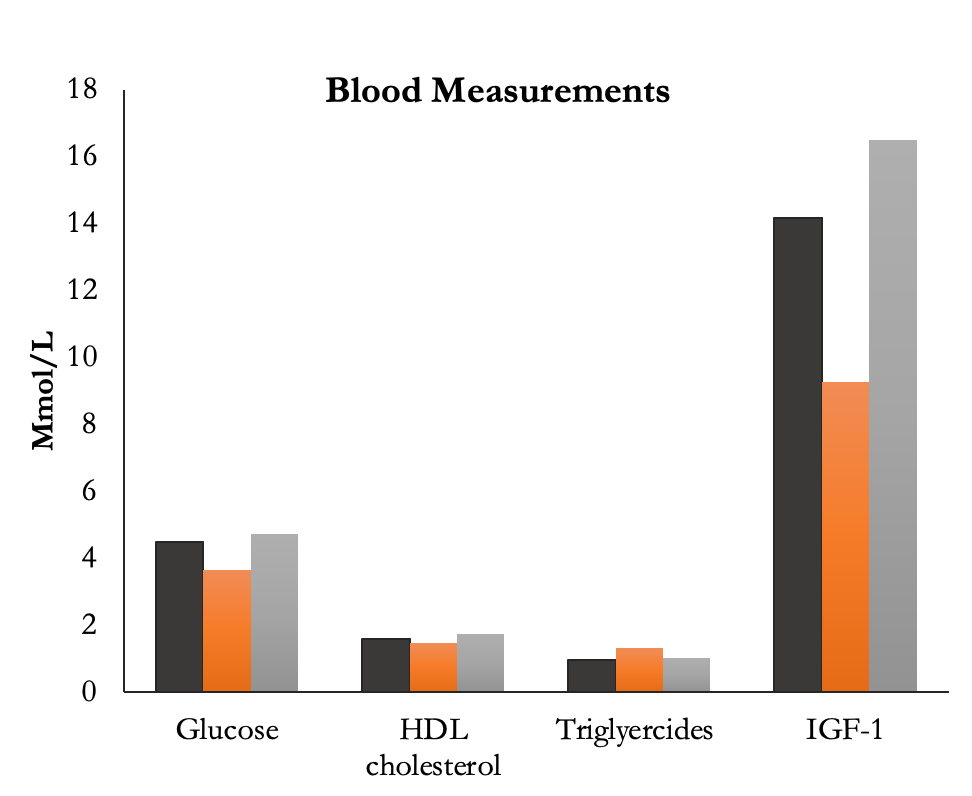
The blood measurements (below) all had significant decreases after 7 days of fasting. Furthermore, at day 60 there was a significant increase compared to baseline for total cholesterol, HDL, and IGF-1.
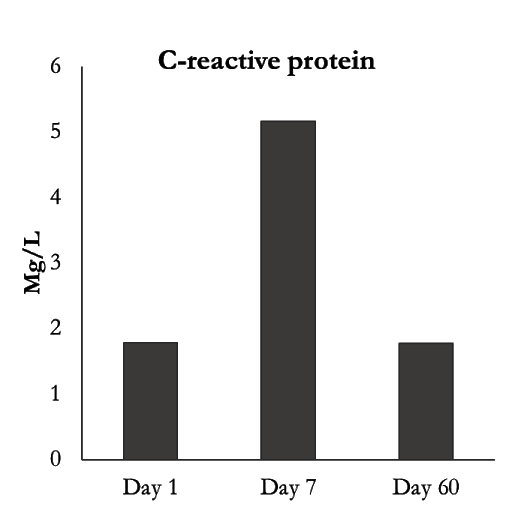
Lastly, something that increased substantially after the 7 day fast was c-reactive protein (CRP) and it returned to baseline at day 60.
The authors do not present data on eating habits and physical activity collected using the questionnaires that were collected.
Author’s Answer
“LDL did not decrease two months after the start of the fast, but there are four further aspects—three of the D60 results and one of the D7 results—that deserve to be highlighted and warrants further research: (1) the maintenance, albeit partial, of weight loss and decreased BMI, accompanied by a possible improvement of body composition, fosters the possible role of periodic fasting in the management of weight loss; (2) the decrease in heart rate, which may reflect an increase in parasympathetic tone [44], is preserved in the medium term; (3) the increase in HDL, which may be an indication of the medium term cardiovascular preventive properties of fasting, is a result corroborated by already suggested trends [16,25]; (4) the behavior of the lipid profile and CRP during fasting has no definitive explication and seems vary in different types of fasting.”
My Answer
Fasting can extend lifespan in bacteria, yeast, worms, and mice. We’re not so sure about the effects in humans because we live much longer than most animals.
In humans, depending upon the amount of physical activity, fasting typically results in a ~20% decrease in serum glucose and decreases in muscle and liver glycogen. This is accompanied by a gradual switch to a metabolic mode where fat-derived ketone bodies and free fatty acids are used as energy sources. The metabolic switch typically occurs in the third phase of fasting when glycogen stores in liver cells are depleted and accelerated adipose tissue lipolysis produces increased fatty acids and glycerol. This happens between 12-36 hours after the start of fasting depending on the liver glycogen content at the beginning of the fast, and on the amount of the individual’s energy expenditure/exercise during the fast.
In 2002, the first guidelines for fasting therapy were published following a conference in Germany and these were recently revised and updated by an expert panel. The most common type of fasting is the Buchinger method, which consists of consuming 250-500kcal usually in the form of liquid (e.g., vegetable juice, broth, and honey) for 5-7 days. If you’re like me then you’re thinking that’s not very intuitive. It’s not fasting at all. It’s just barely above a very low calorie diets (VLCD).
Fasting can be used constantly, known as prolonged fasting, or intermittently, known as intermittent fasting. When it comes to weight loss, continuous and intermittent fasting seem to have very similar results. For example, one study found that overweight participants who dieted for six months using fasting twice a week (500–600 calories on the fasting days) lost fat, displayed improved insulin sensitivity and reduced blood pressure. Importantly this was not different from the continuous energy restriction group (aka normal dieting).
There are a few other studies that have used prolonged fasting with some similar outcomes. A study in participants fasting for 7 days with and without metabolic syndrome found that participants lost ~6kg (5% body weight), had decreases in LDL, no changes in HDL, a decrease in triglycerides, and increases in cortisol as well as CRP. Interestingly the fasting enhanced participants’ mood. It was also well tolerated by all participants. Another study found that fasting as a safe and acceptable procedure that may cause short- and mid-term improvement of increased insulin resistance, but people with type 2 diabetes benefit more than those without it.
Inflammatory markers are frequently increased in obese subjects and weight loss through long-term caloric restriction reduces these biomarkers in women.
The mechanisms behind the clinical effects of fasting are not fully understood, but autophagy is often cited as a major component in the lay press. Autophagy is a housekeeping mechanism that cells in our body use to eliminate damaged organelles, misfolded proteins and pathogens.
A major limitation to this study is the lack of nutrition and training information. The authors even state: “.. finally, because the forms in which the participants reported details on eating habits and physical activity have not yet been analyzed, we cannot conclude in which proportion the observed medium-term changes in clinical parameters are due to the fasting week itself vs. possible habits modification engendered by the fasting experience.” This makes us unable to determine what they were doing (or if they actually adhered) to the fasting period.
How can we apply this?
I chose this study not for its rigor, but for its applicability. This was done at an actual retreat that you can visit. Essentially, this and other data suggest that fasting can be used, without any detriment, as a method to manipulate caloric intake for short periods of time. There is some data indicating it could be used in specific diseases, but more research needs to be done before I’m willing to give a firm conclusion.